Unleashing the Arsenal of Antiplatelet Drugs
Published:
2025-04-07
Atherosclerosis thrombosis is a systemic disease affecting the cardiovascular, cerebrovascular, and peripheral arteries, in which platelet activation and aggregation play an important role in the formation and development of atherosclerosis thrombosis.
Atherosclerosis thrombosis is a systemic disease affecting the cardiovascular and peripheral arteries, in which platelet activation and aggregation play an important role in the development of atherosclerosis thrombosis. Antiplatelet drugs are the cornerstone of the treatment and prevention of cardiovascular events; they achieve antiplatelet aggregation effects through different mechanisms of action.
I. Platelet Thrombosis Process
When vascular endothelial cells are damaged, platelet surface glycoprotein receptors such as GP Ib-IX-V adhere to subendothelial collagen through the action of von Willebrand factor (vWF), forming activated platelets. Subsequently, mediated by GP IIb/IIIa, fibrinogen, through a "bridging" method, binds to different GP IIb/IIIa at both ends, ultimately leading to platelet aggregation. Activated platelets also release endogenous adenosine diphosphate (ADP) and thromboxane A2 (TXA2), ultimately leading to the activation and aggregation of more platelets.
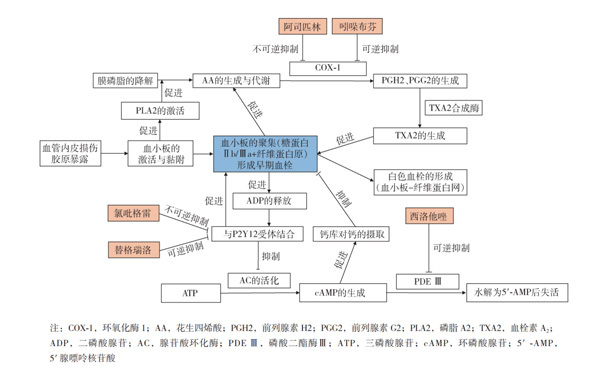
II. Pharmacological Mechanisms of Antiplatelet Drugs
The mechanisms of action of existing antiplatelet drugs often involve preventing the production of second messengers (such as TXA2), inhibiting receptors activated by soluble agonists (such as P2Y12, PAR1), or blocking the binding of fibrinogen and other ligands to GP IIb/IIIa.

Pharmacological Mechanisms of Commonly Used Antiplatelet Drugs
Source: "Expert Consensus on Diagnosis and Treatment of Intolerance and Hyporesponsiveness to Commonly Used Oral Antiplatelet Drugs"
III. Summary of Antiplatelet Drugs
Antiplatelet drugs used clinically mainly include three categories: COX-1 inhibitors, P2Y12 receptor antagonists, and glycoprotein IIb/IIIa (GP IIb/IIIa) receptor antagonists.
1. COX-1 inhibitors
The representative drug is aspirin. Aspirin is a widely used cyclooxygenase inhibitor in the clinic and is the first-line drug recommended by various guidelines for antiplatelet therapy. Aspirin reduces TXA2 synthesis and inhibits platelet aggregation function by directly inhibiting cyclooxygenase (COX-1). However, aspirin has no effect on platelet aggregation caused by other agonists (such as collagen, adenosine diphosphate).
The loading dose of aspirin is 300 mg, and the recommended dose for long-term treatment is 75-100 mg/d. Avoid concomitant use of nonsteroidal anti-inflammatory drugs (such as ibuprofen) as they may affect the antiplatelet effect of aspirin. The risk of bleeding is increased when combined with other antiplatelet and anticoagulant drugs.
2. P2Y12 Receptor Antagonists
Representative drugs include clopidogrel and ticagrelor. Clopidogrel, after metabolism by hepatic cytochrome P450 enzymes, generates an active metabolite that irreversibly inhibits the binding of ADP to the platelet P2Y12 receptor, thereby inhibiting platelet aggregation. Human platelets have three different ADP receptors: P2Y1, P2Y12, and P2X1 receptors; among them, the P2Y12 receptor is the most important in platelet activation. The P2Y12 receptor participates in the process of ADP-induced platelet aggregation, which begins with the activation of the P2Y12 receptor, leading to platelet activation, release, aggregation, and ultimately forming platelet thrombi, playing an important role in primary hemostasis.
Currently, P2Y12 receptor antagonists mainly include thienopyridines (clopidogrel, prasugrel) and non-thienopyridines (ticagrelor), among which ticagrelor is a new reversible P2Y12 receptor antagonist.
In terms of antiplatelet effect strength, ticagrelor is superior to clopidogrel. Prasugrel is a third-generation thienopyridine antiplatelet drug approved by the FDA in 2009. Prasugrel is also a prodrug but only requires one step of conversion by cytochrome P450 enzymes to produce an active metabolite, therefore it takes effect faster.
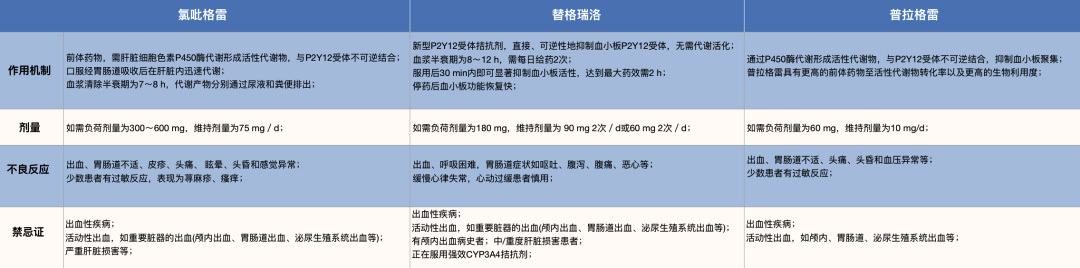
P2Y12 receptor antagonists
Source: "Chinese Expert Consensus on Oral Antiplatelet Drug Treatment for Stable Coronary Artery Disease"
3. Glycoprotein IIb/IIIa (GP IIb/IIIa) Receptor Antagonists
The representative drug is tirofiban. Tirofiban competitively inhibits the binding of fibrinogen and platelet GPIIb/IIIa receptors, inhibiting platelet aggregation. Tirofiban is administered intravenously to prevent thrombus formation after PCI, especially in patients with ST-segment elevation myocardial ischemia.
The main adverse reactions of tirofiban are bleeding and thrombocytopenia. In patients with severe renal insufficiency, its plasma clearance can be reduced by more than 50%. Contraindications should be noted when using it.
4. Other Antiplatelet Drugs
In addition to the commonly used antiplatelet drugs mentioned above, there are some other drugs:
Phosphodiesterase inhibitors, representative drug: cilostazol, dipyridamole;
Thromboxane synthetase inhibitors, representative drug: ozagrel;
Platelet adenylyl cyclase stimulators, representative drug: prostacyclin;
5-hydroxytryptamine receptor antagonists, representative drug: sarpogrelate.
In addition, medical professionals are actively seeking new drug targets, and a series of antiplatelet drugs are undergoing clinical trials, which are expected to provide better treatment options for patients with thrombotic diseases.
References
1. Sun Shuangyong, Jin Jing, Kong Xiaohua, et al. Research progress of antiplatelet drugs and discovery of new target drugs [J]. Drug Evaluation Research, 2021, 44(1):9.
2. Huo Yong, Wang Yongjun, Gu Yongquan, et al. Expert consensus on diagnosis and treatment of intolerance and hyporesponsiveness to commonly used oral antiplatelet drugs [J]. Chinese Journal of Cardiovascular Diseases: Online Edition, 2021(1):13.
3. Anonymous. Chinese expert consensus on oral antiplatelet therapy for stable coronary heart disease [J]. Chinese Journal of Cardiovascular Diseases, 2016, 44(002):104-111.
Keywords:
Learn more about industry trends