Good news for PCI patients - antiplatelet drug testing
Published:
2025-04-07
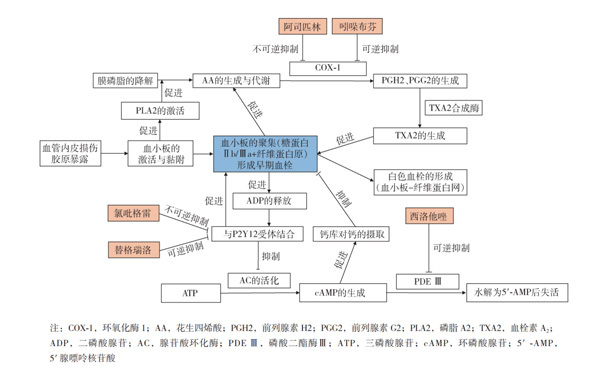
Atherosclerosis thrombosis is the basis of many cardiovascular and cerebrovascular events, and platelets play an important role in the formation and development of atherosclerosis thrombosis.
Atherosclerosis and thrombosis are the basis of various cardiovascular and cerebrovascular events, and platelets play an important role in the development of atherosclerosis and thrombosis. Therefore, antiplatelet drugs have been widely used in primary and secondary prevention of cardiovascular and cerebrovascular diseases to reduce the occurrence of thromboembolic events. However, there are significant differences in the responsiveness of different individuals to antiplatelet therapy, and high platelet reactivity (HPR) has always been an important factor affecting the efficacy of antiplatelet therapy. How to improve the efficacy and safety of antiplatelet drugs and balance the risk of bleeding and thrombotic events has always been a hot topic of clinical concern. In recent years, with the significant increase in the number of PCI cases in China, the importance of optimizing antiplatelet therapy and improving patient prognosis has become increasingly prominent. Platelet function testing (PFT) can be used to assess individual responsiveness to antiplatelet drugs and adjust antiplatelet therapy strategies accordingly, helping to improve the efficacy and safety of antiplatelet therapy.
The 2011 ACCF/AHA/SCAI PCI Guidelines, the 2014 ESC/EACTS Myocardial Revascularization Guidelines, and the 2014 Chinese Expert Consensus on Clinical Testing and Management of Diverse Responses to Antiplatelet Drug Therapy all recommend:
Platelet function testing is recommended to guide antithrombotic therapy for patients with high-risk ACS undergoing PCI who experience re-ischemic events; PCI of high-risk lesions such as left main stem, single-vessel disease, multi-vessel disease; bridging vessel lesions and diffuse lesions requiring overlapping implantation of multiple stents; patients whose clinical and interventional results predict a high risk of thrombosis (such as those with renal insufficiency, diabetes, obesity, dissection during surgery, no-reflow, etc.); and patients whose antiplatelet therapy regimen is planned to be adjusted.
There are currently various methods for platelet function testing, the most common of which are light transmission aggregometry (LTA), point-of-care testing (POCT) methods (e.g., Verify Now), closure time methods (e.g., PFA-100/200), thromboelastography (TEG), intracellular signaling molecule detection (vasodilator-stimulated phosphoprotein, VASP-P), and cell surface activation molecule (P-selectin) methods, etc. These testing methods have been shown by numerous studies to be significantly correlated with adverse clinical events and can be used to assess the efficacy of antiplatelet drugs.
The above-mentioned detection methods have different principles and have their own advantages and disadvantages in practical application. The 2014 European Heart Journal's Expert Consensus on the Application of Platelet Function Testing in Patients After PCI and the 2014 Chinese Expert Consensus on Clinical Testing and Management of Diverse Responses to Antiplatelet Drug Therapy recommend the use of methods with better standardization of Verify Now or VASP detection; if these are unavailable, the LTA method can be used.
Suoce凝 The fully automated platelet aggregometer ( YHK-RPA100 ) is a precise, rapid, and simple antiplatelet therapy testing system. Its principle is microfluidic latex-enhanced immunoturbidimetry, which monitors the efficacy of two major clinically used antiplatelet drugs (COX-1 inhibitors and P2Y12 receptor antagonists) using whole blood samples (no pretreatment), with the simplest operation and fastest time (3-5 min). It guides clinical assessment of risk events (ischemic or bleeding events) during medication, rationalizes medication adjustment, and develops precise, individualized treatment plans.
Keywords:
Learn more about industry trends